Research Paper: Risk assessment and management in obsessive–compulsive disorder by David Veale, Mark Freeston, Georgina Krebs, Isobel Heyman and Paul Salkovskis
For some whose OCD is about very unpleasant or disturbing thoughts it can be challenging to talk about their OCD, worried about how their unwanted thoughts and images might be perceived.
It can be particularly difficult if that person’s OCD involves unwanted intrusive thoughts of a graphic sexual or violent nature. For example, fears about picking up a knife to stab someone, or fears about inappropriately touching a baby or a child, all of which are incredibly common, and do not indicate risk.
As we know, there is no documented evidence suggesting anyone with OCD has actually carried out their actions, far from it, people with OCD go to extreme lengths not to carry out such actions.
But despite worries about sharing such thoughts, it’s important to be honest when talking about our OCD, because health professionals can’t help us if they don’t understand what problems we’re experiencing. Whilst most healthcare professionals should understand how distressing OCD can be and should not be alarmed by the graphic nature of some of those more unpleasant or disturbing thoughts, it would be wrong of us not to say that sadly just very occasionally you may still come across ones that fail to differentiate between OCD and ‘intent’/’risk’. This is not meant to alarm anyone, but we have a duty to educate and prepare you.
This however should not prevent you from reaching out for help and why it’s important we prepare you with some additional tools should you be met with blank expressions or alarmed faces when you open up.
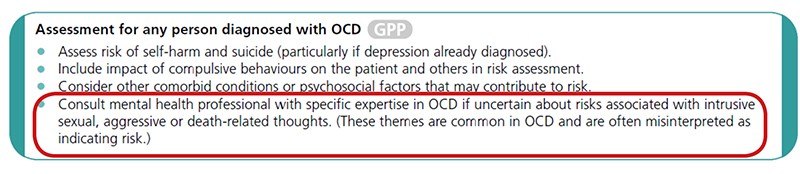
The first thing you should ensure is that the health professional is made aware of is this very specific paragraph in the NHS NICE Guidelines for the treatment of OCD, in which they state: “Consult mental health professional with specific expertise in OCD if uncertain about risks associated with intrusive sexual, aggressive or death-related thoughts. (These themes are common in OCD and are often misinterpreted as indicating risk.)”
As you may remember from our page about obsessions page, such intrusive thoughts are common, even amongst those without OCD as the research published in the OCD book ‘Overcoming Obsessive Thoughts’ by Purdon and Clark showed.
In 2009 OCD specialists Veale, Freeston, Krebs, Heyman and Salkovskis published a paper for health professionals on this very subject, called Risk assessment and management in obsessive–compulsive disorder. If you remain concerned that your health professional is not understanding your OCD then you may wish to refer them to this paper.
In order to make this easier for you, we have included all these references on a special GP Ice-Breaker printout which you can take with you and pass to your GP or the person doing your assessment.
What to read next: